Infrared saunas are a type of sauna that use infrared heaters to emit infrared light, which is then absorbed by the body to produce heat. Unlike traditional saunas, which heat the air around you,...
Jason Ferine Physical Therapy
Blog
7 ANTI-INFLAMMATORY FATS YOU SHOULD EAT, ACCORDING TO A DIETITIAN
Anti-inflammatory foods can help boost your body’s ability to combat inflammation and the diseases it can cause. No matter how many marathons you run, how many dietary supplements you take daily or...
6 FROZEN FOODS A NUTRITIONIST ALWAYS BUYS
Eating a well-balanced diet rich in fruits and vegetables can help protect against many chronic diseases. And yet, nearly 90% of Americans don’t consume the recommended daily amount. The rising...
ARTIFICIAL SWEETENERS CAN HARM SUGAR LEVELS, SHOULDN’T BE ASSUMED SAFE
Artificial sweeteners are a popular way to cut calories and sugar from your diet. They’re found in many products, from drinks to snacks and even some medications. But what do we really know about...
6 HIGH-INFLAMMATORY FOODS
If you’ve ever had an inflammatory condition, such as arthritis or psoriasis, you’ll know that it’s no fun. Inflammation is the body’s response to injury or infection and can cause pain, swelling...
HOW TO START AND MAINTAIN HEALTHY HABITS
Have you ever made a resolution at the beginning of the year only to see yourself scuttling back into your shameful acts just a few months in? Not being able to follow through on our aims makes a...
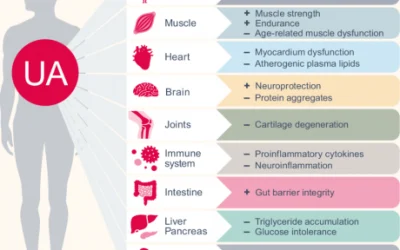
THE CONCEPT OF AGING AND WHY WE LOSE MUSCLE MASS WHEN WE AGE
Scientists investigating gut bacteria have found that the gut bacteria metabolite, UrolithinA holds significant promise of muscle recovery in aging adults. The researchers suggest that UrolithinA...
THE ORIGIN OF PAIN, THE MIND-BODY CONNECTION
Did you know that about 85 percent of back pain and 78 percent of headaches don’t have an identifiable trigger? And, what if I told you that the origin of nearly all physical pain is repressed...
MEDICATIONS AREN’T THE ONLY OPTION.
There are many treatment methods for chronic pain, but the most commonly used are over-the-counter and prescription drugs. But the approaches to treating chronic pain are not limited to medications,...
WANT TO BE PHYSICALLY FIT? WORK UP A SWEAT ONCE A DAY.
According to new research, people who spend more time engaging in physical activity and less time sitting achieve greater overall physical fitness throughout their lifetime. In fact, habitual...
Request An Appointment
Please fill out this form and
we will contact you about scheduling.